Background:
Transcranial doppler (TCD) screening (Sickle Stroke Screening) identifies children ages 2-16 years with sickle cell disease (SCD) at an increased risk for stroke. Significant barriers to undergoing annual screening exist for patients with SCD. Previous studies have shown that individuals from households on public insurance with limited neighborhood opportunity have increased barriers to receiving adequate healthcare, including routine screening; however it is unknown whether low socioeconomic status (SES) influences TCD results.
Methods:
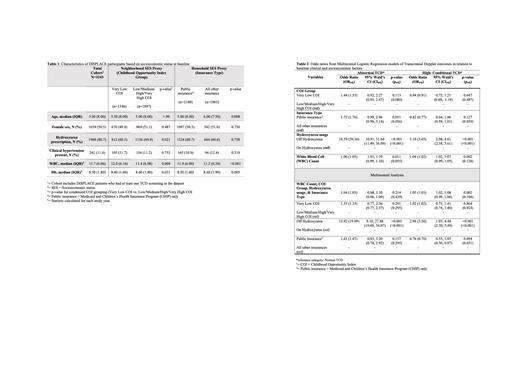
We conducted a secondary analysis of the DISPLACE study, which included a cohort of 3243 TCD-eligible individuals aged 2-16 who had at least one TCD screen performed during their year of study enrollment. We utilized insurance type (Medicaid/CHIP or public versus all other insurances) and overall childhood opportunity index (COI) group (Very Low versus all other COI levels [Low, Medium, High, and Very High]) to proxy household- and neighborhood-level SES. We then examined the association between household- and neighborhood-level SES and conditional and/or abnormal TCD screening results.
Baseline characteristics of the overall cohort (Table 1) were described by COI group and insurance type. The primary outcome was TCD result at baseline (i.e. a patient's first TCD in the database); categorized as abnormal, high-conditional, and normal (reference group). Multinomial logistic regression analysis was used to assess whether clinical (age, sex [female vs. male], hemoglobin (Hgb) level, white blood cell [WBC] count, presence of clinical hypertension [yes, no], hydroxyurea (HU) prescription at baseline [yes, no]) or socioeconomic factors (insurance type and COI group) were independently associated with TCD result. The multinomial regression accounted for age, Hgb level, WBC count, HU prescription, COI group, and insurance type. All tests were two-tailed and, an alpha level of <0.05 and <0.1 (to reduce type II error in logistic regression) were used to determine statistical significance.
Results:
The analytic cohort included 3243 children (Table 1), with 1346 (41.5%) children living in Very Low COI neighborhoods and 2180 (67.2%) of households with public insurance. HU was prescribed to 60.7% of individuals, and this varied by COI level (p=0.021), but not insurance type (p=0.758). WBC count was significantly higher in the Very Low COI group (p=0.004) and public insurance group (p<0.001). Hgb level was noted to be significantly lower in the Very Low COI (p=0.031) and public insurance (p<0.001) groups.
Bivariate logistic regression analysis revealed that COI group (OR 1.53, p=0.08) and insurance type (OR=1.76, p=0.056) were significantly associated at p<0.1 with abnormal TCD outcome individually. Lack of HU prescription was significantly associated at p<0.05 with abnormal TCD result (Odds Ratio [OR]=20.36, p<0.001), and WBC count (OR=1.05, p=0.055) was significantly associated at p<0.1 with abnormal TCD result individually. In the multinomial logistic regression model (included variables listed above), only lack of HU prescription remained significantly associated at p<0.05 with abnormal TCD result (OR=19.09, p<0.001).
Conclusion:
The most robust predictive factor determining abnormal or conditional TCD status in this cohort was lack of HU prescription. Public insurance and COI group as proxies for SES were not independently associated with abnormal or conditional TCD results. As such, the disparities seen by individuals from proxied lower SES are likely mediated by utilization of HU. Notably, HU prescription rates differed by COI group, but not insurance type, suggesting possible neighborhood level factors (such as availability of pharmacies dispensing HU) influencing HU prescription that wouldn't be reflected by insurance type. The limitations of using socioeconomic proxies such as COI group and insurance type must be noted, as these proxies assign group characteristics to an individual based on a snapshot in time, which may not be representative of the dynamic nature of one's SES. Nevertheless, these findings highlight the need to better understand the possible association between SES and HU prescription, as limited HU access and utilization could result in significant health disparities in both treatment and outcomes.
Disclosures
Kanter:Austin Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Vertex: Consultancy, Honoraria; ECOR1: Consultancy; Fulcrum: Consultancy; Bausch: Honoraria; Bluebird Bio: Consultancy; Beam: Consultancy, Honoraria; Guidepoint Global: Consultancy; Chiesi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Watkins, Lourie, Roll&Chance: Consultancy. Archer:Haemonetics: Current equity holder in publicly-traded company, Other: My spouse receives equity as part of his salary; Pfizer: Research Funding; Agios: Research Funding; HHMI: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal